Belgian healthcare faces a data problem hiding in plain sight. Hospitals have spent years digitising patient records, yet most clinical information remains trapped in plain text that cannot be queried, benchmarked, or shared automatically between systems.
To measure the actual state of structured data capture in Belgian hospitals, we surveyed 847 healthcare professionals in May 2025. The respondents span clinical professionals (91%), hospital management (4%), and technical specialists (5%) from regional and university hospitals across Flanders, Brussels, and Wallonia.
The findings reveal a healthcare system that has embraced digital documentation but not yet unlocked its potential. With European Health Data Space requirements approaching in 2027, the gap between current practice and future expectations is wider than many realise.
Key takeaways at a glance
- 56% of clinicians type free text directly into EHRs, making data inaccessible for analysis
- Only 6% report that structured data capture is fully integrated across all their clinical documentation
- 72% of clinical professionals are unfamiliar with EHDS requirements
- Clinicians mention time-consuming data entry (24%) and lack of visible ROI as main adoption barriers
- Only 9% report seamless external data sharing with partners
1. Free text documentation dominates: 56% of clinicians type unstructured notes into EHRs
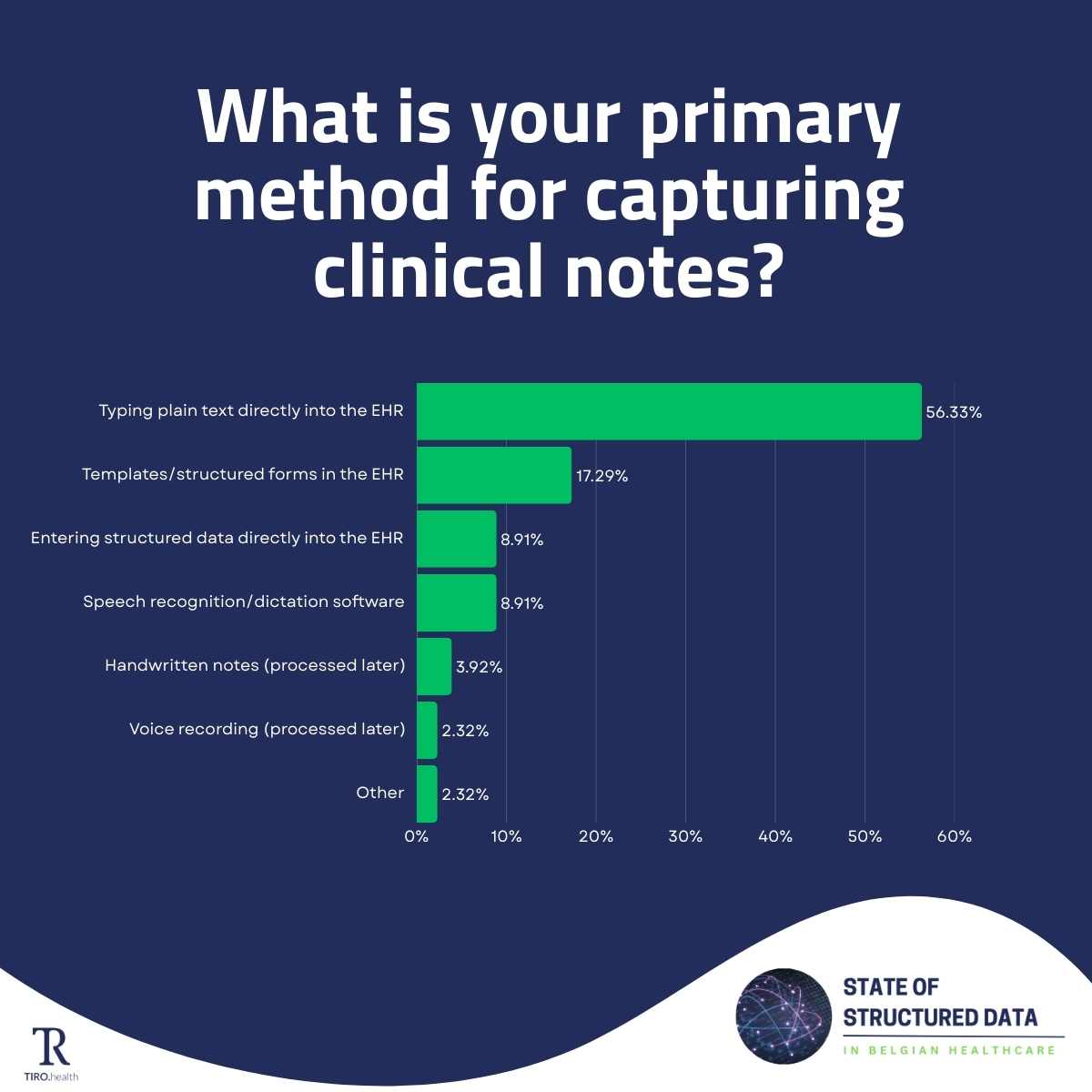
When asked about their primary method for capturing clinical notes, 56% of respondents indicated they type plain text directly into the electronic health record. Only 17% use templates or structured forms, and just 9% enter structured data directly.
Free text documentation cannot be automatically processed for quality measurement, registry reporting, or clinical research. While large language models show promise, they remain insufficiently accurate for reliable clinical data extraction at scale. Moreover, free text cannot enforce completeness: clinicians may simply omit relevant findings, whereas structured templates prompt for required data elements. The result is information that exists in hospital systems but remains essentially invisible to analytical tools.
Speech recognition and dictation software, often positioned as efficiency tools, account for only 9% of primary documentation methods. While these technologies speed up text entry, they typically produce the same unstructured output as typing, leaving the underlying data accessibility problem unsolved.
The technical infrastructure often reinforces these patterns.
Brecht Dekeyser, Director Data & IT at AZ Oostende, describes the current state: "The modules are connected, but insufficiently. Plus everything is still not coded with standards like SNOMED CT."
Even when hospitals have invested in modern EHR systems, the underlying architecture may not support true structured data capture.
2. Structured data integration remains rare: only 6% have achieved complete implementation
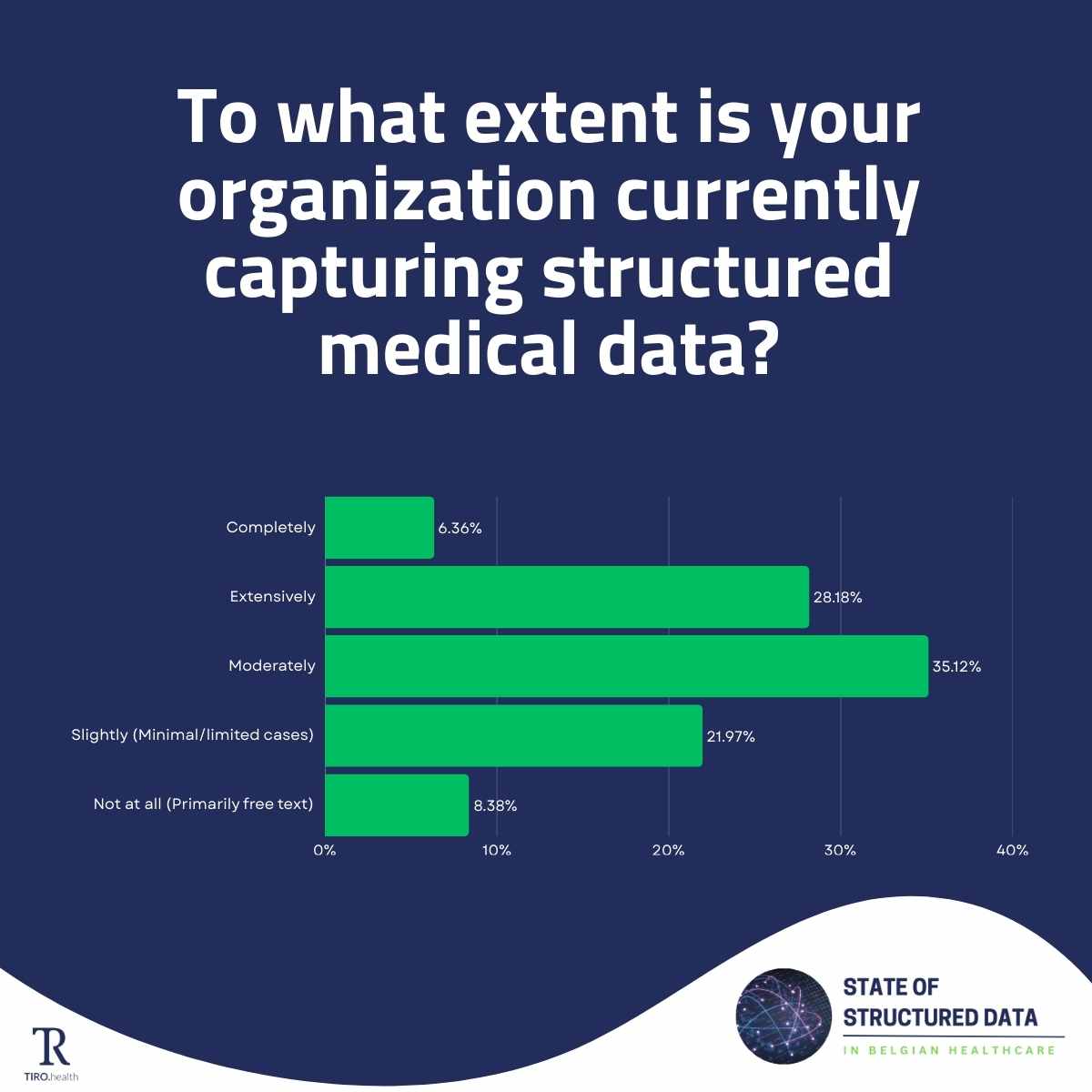
Despite widespread recognition that structured data improves care quality and operational efficiency, actual implementation lags far behind. When asked to what extent their organisation captures structured medical data, only 6% of clinical professionals and 5% of technical specialists reported complete integration across all documentation.
The majority remain stuck in partial adoption. About 35% of clinical professionals describe their structured data capture as moderate but inconsistent across departments. Another 22% report only slight implementation in limited cases. And 8% still rely primarily on free text with minimal structured elements.
This pattern suggests that the challenge is not awareness but execution. Healthcare organisations understand the value of structured data for quality improvement and research. They struggle to move from pilot projects and isolated use cases to systematic, organisation-wide implementation.
3. Healthcare data sharing between organisations remains severely limited
The shift toward value-based healthcare demands data that flows between organisations. Quality registries aggregate outcomes across hospitals to measure what actually works. Research networks pool patient data for multicentric clinical studies. Care coordination requires information to follow patients across settings and providers.
Yet our survey found that only 9% of respondents report complete, seamless data sharing with authorised external partners. Another 19% share most data via standard protocols extensively. The remaining 72% face moderate to severe limitations in healthcare interoperability.
Nearly 12% cannot share structured medical data externally at all. Another 29% manage only basic sharing with significant barriers. And 31% share data with select partners through custom, often manual processes that do not scale.
For Belgian hospitals aiming to participate in multicentric research, contribute to national quality registries, or collaborate within hospital networks, these interoperability limitations create real obstacles that consume time and resources with every data request. With EHDS requirements approaching in 2027, these manual workarounds will no longer be sustainable.
4. Documentation burden and poor tooling block structured data adoption
Healthcare professionals do not need convincing that better data leads to better care. They need tools that capture structured information without adding to their clinical documentation burden.
Time concerns dominate the obstacle list. When asked about the main barriers to effective structured data capture, 24% cited time-consuming data entry processes. Another 24% specifically mentioned concerns about time spent on documentation versus patient care. These numbers suggest that efficiency is non-negotiable for clinical adoption.
Lack of user-friendly data entry tools ranks third at 18%, followed by EHR integration issues at 15%. Interestingly, only 6% of clinical professionals cite staff resistance as a primary barrier, though management perceives this resistance more strongly at 15%.
But time constraints alone do not explain the adoption gap. There is a deeper question that clinicians ask themselves before investing effort in structured documentation.
When documentation effort never translates into visible benefits, adoption stalls regardless of how streamlined the process becomes. In one case we encountered, a specialist had been entering structured data for seven months without ever receiving access to the resulting dashboard. The promised insights never materialised, and motivation understandably declined.
"The switch to electronic systems has simply made everything less efficient for physicians. A paper prescription was just a sheet, you put an illegible scribble on it, and you're done. Electronically you have to select it, you have to fill in fields, those are the steps." Brecht Dekeyser, Director Data & IT at AZ Oostende
This observation highlights a fundamental tension. Structured data capture adds steps to workflows that clinicians previously completed quickly, even if imperfectly. The long-term benefits of queryable, shareable data do not offset the immediate friction unless organisations deliberately close the feedback loop.
5. EHDS readiness: 72% of clinicians unfamiliar with European Health Data Space requirements
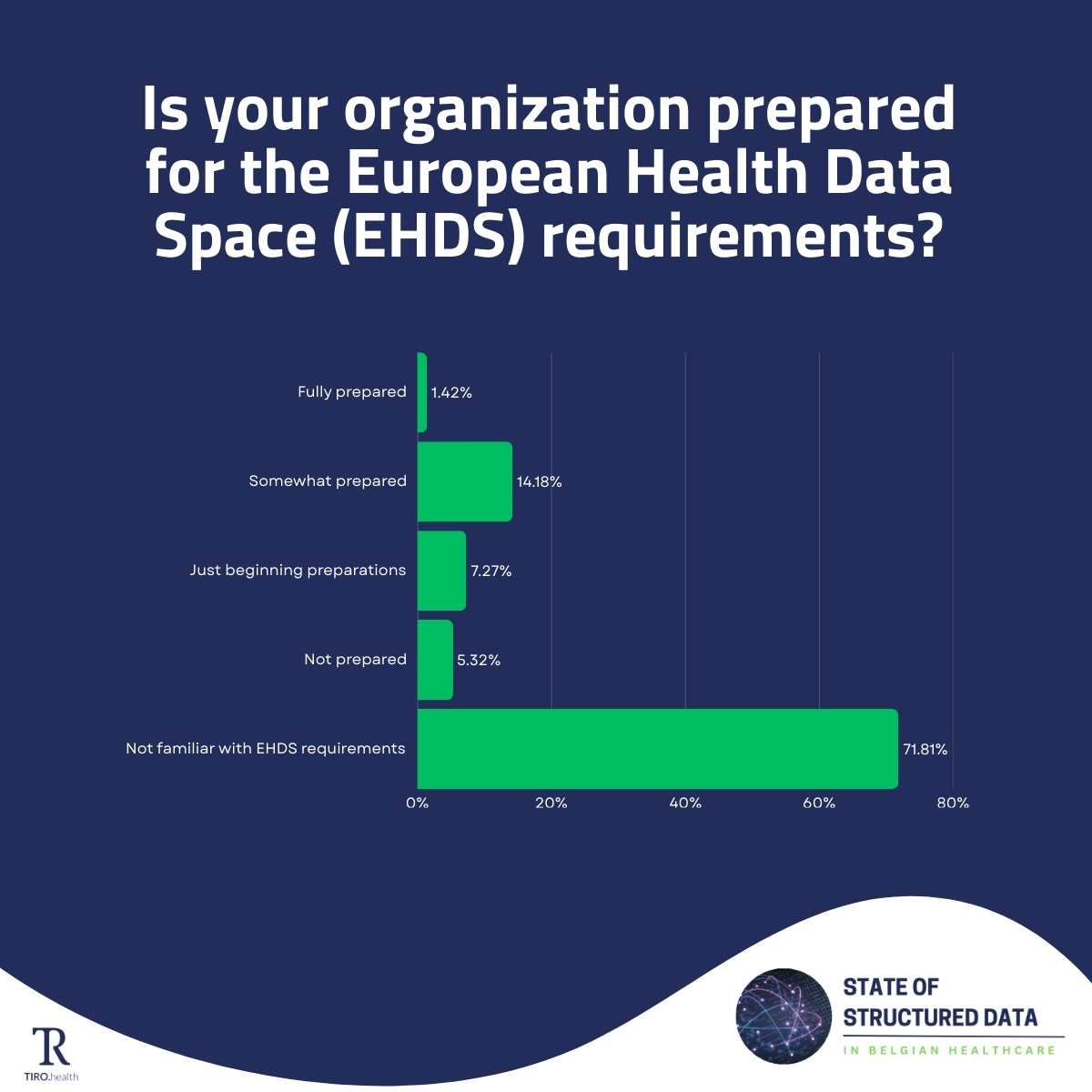
Management and technical specialists show better awareness. Among directors, 43% describe their organisation as somewhat prepared and 14% as fully prepared. But even in these groups, significant portions remain unfamiliar with what EHDS compliance will require.
The responsibility question adds complexity. Many hospitals assume that EHR vendors will deliver compliance automatically through system updates. Yet hospitals will ultimately be accountable for the quality and structure of data they submit.
The gap between current structured data practices and EHDS expectations is significant. Organisations building structured data capabilities now gain a head start. Those waiting for 2027 will find themselves catching up under pressure.
AI as accelerator, not replacement
Given the documentation burden clinicians face, artificial intelligence offers an obvious potential solution. Our survey found that 50% of clinical professionals remain unsure about AI for clinical documentation, while technical specialists show more enthusiasm with concrete implementation plans.
The trust question is telling. When asked how much they would trust an AI-generated draft of clinical documentation, only 2% indicated complete trust. Another 25% expressed high trust, but the majority remains cautious or uncertain.
This caution is not technophobia. It reflects a reasonable position that healthcare professionals across Belgian hospitals share.
But even the efficiency gains deserve scrutiny. Brecht Dekeyser, whose hospital is piloting ambient AI with psychologists, oncology nurses, and some physicians, offers a nuanced view:
"I don't think it saves that much time, honestly. It's about personal contact. You still have to review AI output."
The implication for AI adoption in healthcare documentation is clear. Tools that generate drafts for human review will find acceptance. Tools that claim to eliminate the need for clinical oversight will face resistance, and rightly so. The path forward combines AI efficiency with human accountability.
What this means for Belgian healthcare
These five findings paint a consistent picture. Belgian healthcare has digitised documentation without yet transforming it. Information flows into electronic systems but remains locked in formats that limit its utility. The tools and workflows needed for structured data capture exist but have not reached the clinicians who generate most patient information.
The path forward requires closing these gaps before external pressure forces rushed solutions. Hospitals that build structured data capabilities now gain immediate benefits in quality measurement and research participation while preparing for regulatory requirements ahead.
The question is no longer whether structured data matters. It is whether healthcare organisations will invest proactively or wait until compliance deadlines and competitive pressure force their hand.
Frequently asked questions
What is structured data in healthcare?
Structured data refers to clinical information captured in standardised, coded formats that computers can automatically process. Unlike free text notes, structured data can be queried for quality measurement, aggregated for research, and shared between healthcare systems without manual interpretation.
Why do Belgian hospitals struggle with structured data capture?
The main barriers are practical: time-consuming data entry (24%), concerns about documentation time versus patient care (24%), and lack of user-friendly tools (18%). Additionally, many clinicians do not see tangible benefits from their documentation efforts, reducing motivation to use structured formats.
What is the European Health Data Space (EHDS)?
The EHDS is EU legislation requiring healthcare organisations to share health data in standardised, interoperable formats. Enforcement will start in 2027. The regulation aims to enable cross-border healthcare, facilitate research, and give patients control over their health data.
How prepared are Belgian hospitals for EHDS 2027?
Our research shows significant gaps. Among clinical professionals, 72% are not familiar with EHDS requirements. Only 1.4% consider their organisation fully prepared. Management shows better awareness, but even there, substantial work remains before the approaching deadline.
What percentage of clinical data is unstructured in Belgium?
Our survey found that 56% of Belgian clinicians primarily use free text when documenting patient encounters. Broader research suggests that up to 87% of clinical information in electronic health records remains unstructured and difficult to analyse.
About the study
This survey represents the most comprehensive assessment of structured data practices in Belgian healthcare to date. Conducted by Tiro.health in May 2025, with distribution support from HOGENT and validation by Delaware consulting and the European Institute for Innovation through Health Data, the research captured responses from 847 professionals across all Belgian regions and healthcare settings.
Click here for the complete report with detailed breakdowns by region, hospital type, and specialty